Topic 2 DQ 1 Muscarinic Antagonist (Atropine)
Choose either a muscarinic agonist or antagonist agent and provide an appropriate indication for use. Share the mechanism of action of this medication and hints for monitoring, side effects, and drug interactions, including interactions with CAM, ethnic, cultural, and genetic differences.
What other considerations need to be made when prescribing these medications in relation to other systems and receptors? Include the name of the medication in the subject line so that the medications can be followed. Include references using APA format.
Download Sample DQ response: To ensure you answer all aspects of the DQ posts I request that you set your responses up with headings signifying each aspect of the prompt. Here is a sample of what I mean, points will be deducted for not answering all aspects of the DQ.
Muscarinic Antagonist (Atropine)
Ethacrynic Acid (Edecrin): Loop Diuretic (PDR, 2021).Mechanism of action: Ethacrynic acid primarily acts to inhibit the reabsorption of sodium and chloride in the ascending limb of the loop of Henle (PDR, 2021).
Monitoring: Cr at baseline; BUN/Cr, serum CO2, electrolytes frequently early in treatment then periodically during active diuresis, cardiac monitoring, weight gain or loss, vital signs (Epocrates, 2021).
Side Effects: Hypotension, hypovolemia, orthostatic hypotension, sympathectomy, syncope, acid/base imbalance, dehydration, electrolyte imbalance, hypocalcemia, hypochloremia, hypokalemia, hypomagnesemia, metabolic alkalosis. Greater risk of ototoxicity when compared to other loop diuretics (Epocrates, 2021).
Muscarinic Antagonist (Atropine)
Severe Adverse Reactions: Agranulocytosis, pancreatitis hearing loss, GI bleeding, azotemia, oliguria (PDR, 2021).CAM Interactions:Dong quai, licorice, magnesium, potassium, St. John’s wort, vitamin B1 (EBSCO, 2019).
Positive or Negative experience with Ethacrynic acid: This author has not yet had any experience with Ethacrynic acid specifically but has had experiences with patients not taking other loop diuretics such as their Furosemide especially when traveling as they did not want to constantly have to stop to urinate; because of this inconvenience patients would have an exacerbation of their congestive heart failure and present to the emergency department most commonly with chest pain, shortness of breath, or painful extremity swelling.
Patients that were placed on diuretics, especially IV diuretics were made fall risk patients due to potential hypotension, electrolyte imbalance, IV lines, and risk of getting out of bed without assistance.
Muscarinic Antagonist (Atropine)
Evidence and Treatment Guidelines: 64 y/o African American woman, no comorbid issues.Loop diuretics should be avoided when less efficacious diuretics (thiazides) will suffice.
Conditions that justify the use of loop diuretics such as furosemide include:
(1) pulmonary edema associated with congestive heart failure (CHF)
(2) edema of hepatic, cardiac, or renal origin that has been unresponsive to less efficacious diuretics
(3) hypertension that cannot be controlled with other diuretics.
Muscarinic Antagonist (Atropine)
Furosemide is especially useful in patients with severe renal impairment because, unlike the thiazides.This drug class can promote diuresis even when renal blood flow and glomerular filtration rate (GFR) are low. If treatment with loop diuretics alone is insufficient, a thiazide diuretic may be added to the regimen. There is no benefit to combining furosemide with another loop diuretic (Rosenthal & Burchum, 2021).
Muscarinic Antagonist (Atropine)
Geriatric patients: According to the Beers Criteria, diuretics are considered potentially inappropriate medications (PIMs) in geriatric patients and should be used with caution due to the potential for causing or exacerbating SIADH or hyponatremia.
Sodium levels should be closely monitored when starting or changing dosages of diuretics in older adults (PDR, 2021).African American race is associated with significantly greater systolic BP (SBP) and/or diastolic BP (DBP) responses to thiazide and loop diuretics compared to European-American patients in small studies (Fuentes et al., 2013). EBSCO CAM Review Board. (2019). Loop diuretics (drug interactions).
Salem Press Encyclopedia of Health.Ethacrynic Acid. (2021, June). https://online.epocrates.com/drugs/67901/Edecrin/Adult-Dosing Ethacrynic Acid. (2021, June). https://www.pdr.net/drug-summary/Edecrin-Sodium-Edecrin-ethacrynate-sodium—-ethacrynic-acid-2065Fuentes, L., Sung, J. Y., Schwander, K. L., Kalathiveetil, S., Hunt, S. C., Arnett, D. K., & Rao, D. C. (2013). The role of SNP-loop diuretic interactions in hypertension across ethnic groups in HyperGEN. Frontiers in Genetics, 4. https://doi-org.lopes.idm.oclc.org/10.3389/fgene.2013.00304Rosenthal, L. D., & Burchum, J. R. (2021). Lehne’s pharmacotherapeutics for advanced practice nurses and physician assistants. Elsevier.
ALSO CHECK: Topic 2 DQ 2 Adrenergic Agonist or Antagonist
ORDER A PLAGIARISM-FREE PAPER HERE !!
Solution
Muscarinic Antagonist (Atropine)
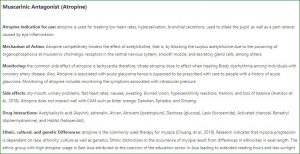
Atropine indication for use: atropine is used for treating low heart rates, hypersalivation, bronchial secretions, used to dilate the pupil, as well as a pain reliever caused by eye inflammation.
Mechanism of Action: Atropine competitively hinders the effect of acetylcholine, that is, by blocking the surplus acetylcholine due to the poisoning of organophosphorus at muscarinic cholinergic receptors in the central nervous system, smooth muscle, and secretory gland cells, among others.
Monitoring: the common side effect of atropine is tachycardia therefore, titrate atropine dose to effect when treating Brady dysrhythmia among individuals with coronary artery disease. Also, Atropine is associated with acute glaucoma hence is supposed to be prescribed with care to people with a history of acute glaucoma. Monitoring of atropine includes monitoring the symptoms associated with intraocular pressure. Muscarinic Antagonist (Atropine).
Side effects: dry mouth, urinary problems, fast heart rates, nausea, sweating, blurred vision, hypersensitivity reactions, tremors, and loss of balance (Avetisov et al., 2018). Atropine does not interact well with CAM such as bitter orange, Danshen, Ephedra, and Ginseng. Muscarinic Antagonist (Atropine).
Drug interactions: Acetylsalicylic acid (Aspirin), adrenalin, Ativan, Atrovent (ipratropium), Dextrose (glucose), Lasix (furosemide), Activated charcoal, Benadryl (diphenhydramine), and Haldol (haloperidol). Muscarinic Antagonist (Atropine).
Ethnic, cultural, and genetic Differences: atropine is the commonly used therapy for myopia (Chuang, et al., 2019). Research indicates that myopia progression is dependent on race, ethnicity, culture as well as genetics. Ethnic distinctions in the occurrence of myopia result from differences in ethnicities in axial length.
The ethnic group with high atropine usage in East Asia attributed to the coercion of the education sector in Asia leading to extended reading hours and less sunlight exposure, a risk factor for myopia (Luong et al., 2020). Myopia is a genetic condition as it involves hundreds of genes. There is a greater risk of having myopia if the immediate relatives had or have myopia as compared to non-infected individuals. Therefore the high rate of atropine usage among such individuals.
Other Considerations: there are several considerations physicians should observe when prescribing atropine including patient’s apical pulse before dosage administration, age as old adults are prone to CNS disturbances, an infant’s temperature when prescribing to an infant, monitor GI motility of the patient, the drug interaction in case a patient is on another medication and drug contradictions.
Muscarinic Antagonist (Atropine)
References
Avetisov, S. E., Fisenko, V. P., Zhuravlev, A. S., & Avetisov, K. S. (2018). Atropine is used for the prevention of myopia progression. Vestnik Oftalmologii, 134(4), 84-90.
Luong, T. Q., Shu, Y. H., Modjtahedi, B. S., Fong, D. S., Choudry, N., Tanaka, Y., & Nau, C. L. (2020). Racial and ethnic differences in myopia progression in a large, diverse cohort of pediatric patients. Investigative ophthalmology & visual science, 61(13), 20-20.
Wu, P. C., Chuang, M. N., Choi, J., Chen, H., Wu, G., Ohno-Matsui, K., … & Cheung, C. M. G. (2019). Update in myopia and treatment strategy of atropine use in myopia control. Eye, 33(1), 3-13.
